Abstract
Mini Review
Bleeding complications at the access sites during catheter directed thrombolysis for acute limb ischaemia: Mini review
Elias Noory*, Tanja Böhme, Ulrich Beschorner and Thomas Zeller
Published: 03 March, 2021 | Volume 5 - Issue 1 | Pages: 001-003
Acute and subacute ischemia of the lower limbs represents a major emergency with a high in-hospital mortality, complication, and leg amputation rates.
Treatment options for acute limb ischemia include systemic anticoagulation, followed by various catheter based options including infusion of fibrinolytic agents (pharmacological thrombolysis), pharmacomechanical thrombolysis, catheter-mediated thrombus aspiration, mechanical thrombectomy, and any combination of the above or open surgical intervention (thromboembolectomy or surgical bypass).
Minor and major bleeding complication during catheter directed thrombolysis (CDT) especially at access site are frequent. Bleeding complications require often an interruption or termination of CDT affecting clinical outcome of the patients. Recently we examined a new access site bleeding protection device during CDT.
Read Full Article HTML DOI: 10.29328/journal.avm.1001014 Cite this Article Read Full Article PDF
Keywords:
Acute limb ischemia; Peripheral artery disease; Thrombectomy; Catheter directed thrombolysis; Protection device; Bleeding complications
References
- Ouriel K, Shortell CK, De Weese JA, Green RM, Francis CW, et al. A comparison of thrombolytic therapy with operative vascularization in the initial treatment of acute peripheral arterial ischemia. J Vasc Surg. 1994; 19: 1021–1030. PubMed: https://pubmed.ncbi.nlm.nih.gov/8201703/
- Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischaemia of the lower extremity. The STILE trial. Ann Surg. 1994; 220: 251–268. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1234376
- Ouriel K, Veith FJ, Sasahara AA. Thrombolysis or peripheral arterial surgery: phase I results. TOPASInvestigators.J Vasc Surg. 1996; 23: 64-73. PubMed: https://pubmed.ncbi.nlm.nih.gov/8558744/
- Diffin DC, Kandarpa K. Assessment of peripheral intra-arterial thrombolysis versus surgical revascularization in acute lower-limb ischemia: a review of limb-salvage and mortality statistics. J Vasc Interv Radiol. 1994; 7: 57–63. PubMed: https://pubmed.ncbi.nlm.nih.gov/8773976/
- Beyersdorf F, Matheis G, Kruger S. Avoiding reperfusion injury after limb revascularization: experimental observations and recommendations for clinical application. J Vasc Surg. 1989; 9: 757–766.
- Robertson I, Kesse DO, Berridge DC. Fibrinolytic agents for peripheral arterial occlusion. Cochrane Database Syst Rev. 2013; 12: CD001099. PubMed: https://pubmed.ncbi.nlm.nih.gov/24357258/
- Ebben HP, Jongkind V, Wisselink W, Hoksbergen A, Yeung KK. Catheter Directed Thrombolysis Protocols for Peripheral Arterial Occlusions: a Systematic Review European Journal of Vascular & Endovascular Surgery, Eur. J.Vasc. Endovasc. Surg. 2019; 57: 667-675. PubMed: https://pubmed.ncbi.nlm.nih.gov/31005512/
- Verhamme P, Heye S, Peerlinck K, Cahillane G, Tangelder M, et al. Catheter-directed thrombolysis with microplasmin for acute peripheral arterial occlusion (PAO): an exploratory study. Int Angiol. 2012; 31: 289–296. PubMed: https://pubmed.ncbi.nlm.nih.gov/22634985/
- Kühn JP, Hoene A, Miertsch M, Traeger T, Langner S, et al. Intraarterial Recombinant Tissue Plasminogen Activator Thrombolysis of Acute and Semiacute Lower Limb Arterial Occlusion: Quality Assurance, Complication Management, and 12-Month Follow-Up Reinterventions. Am J Roentgenol. 2011; 196: 1189–1193. PubMed: https://pubmed.ncbi.nlm.nih.gov/21512091/
- Grip O, Kuoppala M, Acosta S, Wanhainen A, Åkeson J, et al. Outcome and complications after intra-arterial thrombolysis for lower limb ischaemia with or without continuous heparin infusion. Br J Surg. 2014; 101: 1105–1112. PubMed: https://pubmed.ncbi.nlm.nih.gov/24965149/
- Plate G, Jansson I, Forssell C, Weber P, Oredsson S. Thrombolysis for Acute Lower Limb Ischaemia—A Prospective, Randomised, Multicentre Study Comparing Two Strategies. Eur J Vasc Endovasc Surg. 2006; 31: 651–660. PubMed: https://pubmed.ncbi.nlm.nih.gov/16427339/
- Ricco JB, Schneider F. Angio-Seal hopes for antegrade puncture require better evidence. Eur J Vasc Endovasc Surg. 2014; 48: 226–227. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24951375
- Noory E, Beschorner U, Zeller T, Böhme T. A new protection system to avoid major bleeding at puncture sites -results from the first in men study. Cardiol Cardiovasc Med. 2000; 4: 717-728.
Figures:

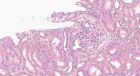
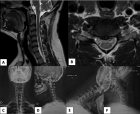
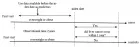
Figure 1
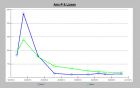
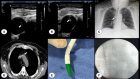
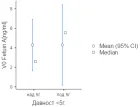
Figure 2
Similar Articles
-
Clinical characteristics in STEMI-like aortic dissection versus STEMI-like pulmonary embolismOscar MP Jolobe*. Clinical characteristics in STEMI-like aortic dissection versus STEMI-like pulmonary embolism. . 2020 doi: 10.29328/journal.avm.1001013; 4: 019-030
-
Bleeding complications at the access sites during catheter directed thrombolysis for acute limb ischaemia: Mini reviewElias Noory*,Tanja Böhme,Ulrich Beschorner,Thomas Zeller. Bleeding complications at the access sites during catheter directed thrombolysis for acute limb ischaemia: Mini review. . 2021 doi: 10.29328/journal.avm.1001014; 5: 001-003
Recently Viewed
-
Dairy cattle producers’ perception on Oestrus Synchronization and mass artificial insemination services in Waliso and Ilu Districts of South West Shoa Zone of Oromia, EthiopiaAbera Fekata*,Ulfina Galmessa,Lemma Fita,Chala Merera,Amanuel Bekuma. Dairy cattle producers’ perception on Oestrus Synchronization and mass artificial insemination services in Waliso and Ilu Districts of South West Shoa Zone of Oromia, Ethiopia. Insights Vet Sci. 2020: doi: 10.29328/journal.ivs.1001020; 4: 010-013
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The prognostic value of p53 and WT1 expression in cancer: new molecular insights and epigenetics explanations lead to a new medical hypothesisAhed J Alkhatib* and Ilham Ahed Alkhatib. The prognostic value of p53 and WT1 expression in cancer: new molecular insights and epigenetics explanations lead to a new medical hypothesis. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001034; 7: 003-009
-
Anticancer Activity of Genistin: A Short ReviewMd Mizanur Rahaman*, Md Iqbal Sikder, Muhammad Ali Khan and Muhammad Torequl Islam. Anticancer Activity of Genistin: A Short Review. Arch Cancer Sci Ther. 2023: doi: 10.29328/journal.acst.1001035; 7: 010-013
-
Knowledge, Attitude, and Practice of Healthcare Workers in Ekiti State, Nigeria on Prevention of Cervical CancerAde-Ojo Idowu Pius*, Okunola Temitope Omoladun, Olaogun Dominic Oluwole. Knowledge, Attitude, and Practice of Healthcare Workers in Ekiti State, Nigeria on Prevention of Cervical Cancer. Arch Cancer Sci Ther. 2024: doi: 10.29328/journal.acst.1001038; 8: 001-006
Most Viewed
-
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trialSathit Niramitmahapanya*,Preeyapat Chattieng,Tiersidh Nasomphan,Korbtham Sathirakul. Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial. Ann Clin Endocrinol Metabol. 2023 doi: 10.29328/journal.acem.1001026; 7: 00-007
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001030; 8: 004-012
-
Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging PresentationKarthik Baburaj*, Priya Thottiyil Nair, Abeed Hussain, Vimal MV. Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging Presentation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001029; 8: 001-003
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023 doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The benefits of biochemical bone markersSek Aksaranugraha*. The benefits of biochemical bone markers. Int J Bone Marrow Res. 2020 doi: 10.29328/journal.ijbmr.1001013; 3: 027-031

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."